
Carol Smiljan/NurPhoto via Getty Images
- Vaccine research and development has improved massively throughout history.
- Nearly 200 years passed between the creation of the first successful vaccine and the eventual eradication of smallpox.
- The influenza virus was isolated in a lab in 1933, and the first flu vaccine wasn’t licensed until 1945.
- Coronavirus vaccine research began just a few months after the first case of COVID-19 was observed, and it has progressed at a rapid pace.
- Visit Business Insider’s homepage for more stories.
Research to develop a vaccine for the novel coronavirus has taken place at a historically fast pace, with clinical trials kicking off just a few months after the first case was identified.
Rollout for high-risk groups could begin as soon as December 2020, although the vaccine won’t be widely available until spring or summer 2021.
In comparison, the influenza virus was first isolated in a lab in 1933, and an effective flu vaccine was not licensed until 1945. Many technological advances, like the invention of the bifurcated (two-pronged) needle for more efficient vaccine delivery in 1965, have improved vaccines since the early days of research.
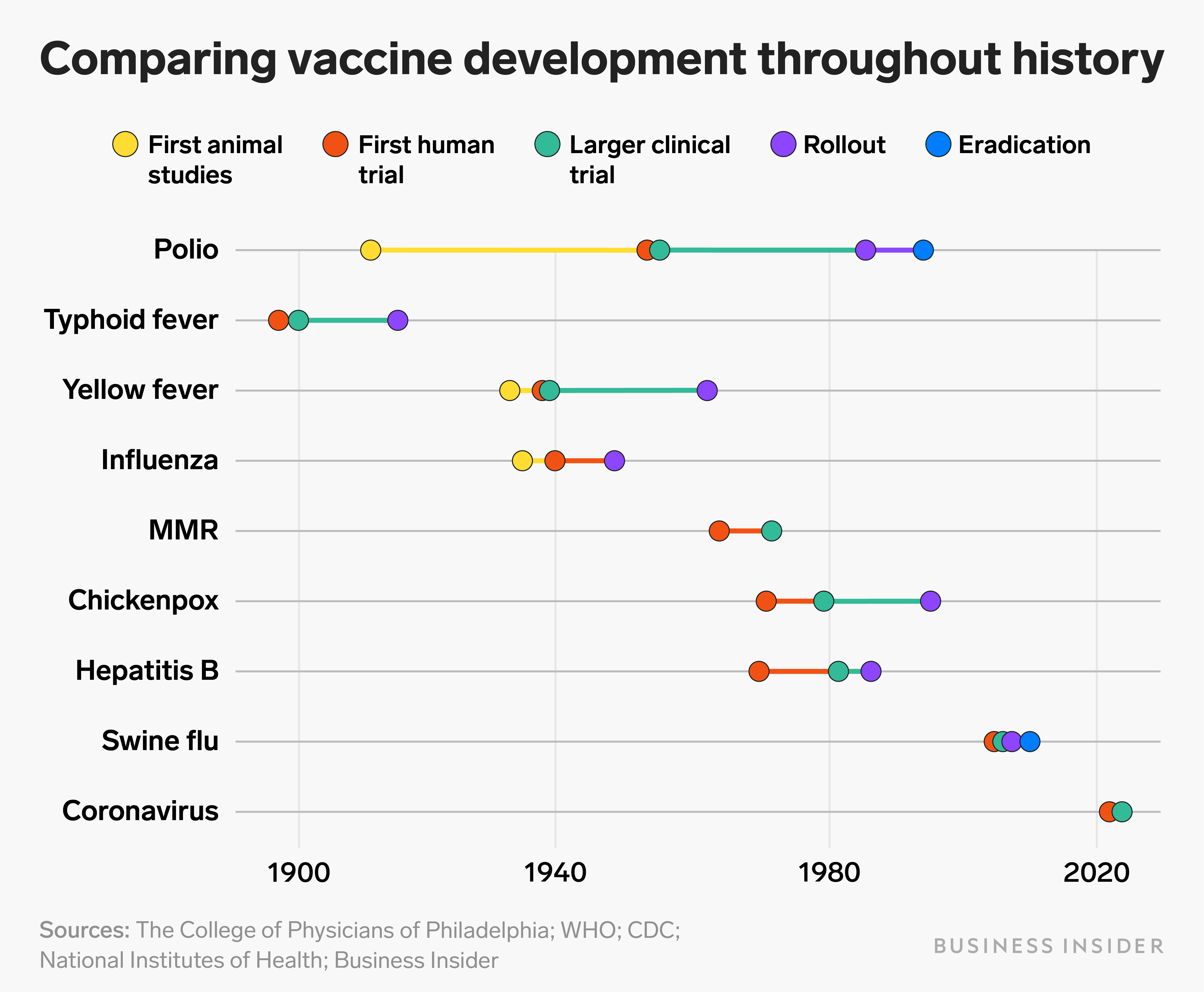
Business Insider compiled timelines of vaccine development throughout history, from polio to swine flu, to demonstrate how the pace of research has evolved.
The first vaccine was created in the 1700s
In 1796, British physician Edward Jenner successfully tested the first smallpox vaccine by injecting a young boy with a milder, smallpox-like disease that typically affected cows. He wrote to the Royal Society of Medicine detailing his experiment, but they rejected his paper.
Jenner tested the vaccine on 22 more patients and self-published his results in a pamphlet in 1798, which was met with mixed reviews. But news of the vaccine quickly spread after another doctor, Henry Cline, successfully replicated Jenner's results.
No advisory committee existed to test the safety and efficacy of the vaccine at the time, so Jenner was free to provide the vaccine to anyone who requested it. Vaccine material reached most European countries by 1800, and in 1802, Dr. Benjamin Waterhouse performed a public test of vaccination in Boston. The city's board of health sponsored the trial and 19 volunteers were successfully vaccinated.
Smallpox became the first infectious disease to be completely eradicated by a vaccine in 1980, following advancements in needle technology and a push for mass vaccinations by the World Health Organization.
That centuries-long endeavor paved the way for many more vaccines to come, and many more public-health successes leading up to the current efforts to quell the coronavirus pandemic.
Polio
Scientists began investigating polio immunity at the Rockefeller Institute for Medical Research in New York in the early 20th century. In 1910, Simon Flexner saw that monkeys who survived polio had developed antibodies.
However, the first two polio vaccine trials in humans in 1935 had disastrous results. The trials involved a combined total of about 21,000 children. Several of them died of polio, and many others were paralyzed or experienced allergic reactions.
Nearly two decades later, in 1952, Jonas Salk developed a vaccine made with killed polio virus. His early trial results confirmed that the vaccine triggered antibody production. But in interviews Salk cautioned that it would take time for larger trials to prove safety and efficacy. He even went on the radio to address overly optimistic media reports.
In 1955, Salk's polio vaccine was found to be 80-90% effective in a randomized, double-blind clinical trial involving 1.3 million children. The US government licensed the vaccine, but the Surgeon General suspended rollout when some batches of the vaccine were found to contain live polio virus. Over 260 cases of polio were attributed to vaccines produced by Cutter Laboratories, prompting an increase in government oversight.
Polio vaccinations resumed in the fall of 1955, and the Pan American Health Organization eventually declared polio eradicated from the Americas in 1994.
Typhoid fever
Several groups were researching a vaccine for typhoid fever in the 1890s, and credit for the discovery is shared among Richard Pfeiffer and Wilhelm Kolle in Germany and Almroth Wright in the UK.
Wright tested his vaccine in 1896: first on two Indian medical officers, then on himself and his co-investigator, and finally on 15 British soldiers. After Wright's vaccine was proven effective, it was first rolled out to the British Army in 1899. Nearly 15,000 soldiers were immunized, successfully lowering rates of typhoid fever among the troops.
The US Army implemented mandatory vaccinations in 1911, and the typhoid vaccine was made available to the American public in 1914. Nowadays, Americans are only recommended to get vaccinated if they're traveling to an area where typhoid is endemic. Vaccination campaigns are still underway in some South Asian and African countries.
Yellow fever
In 1931, Harvard virologist Max Theiler demonstrated that mice injected with serum from previously infected monkeys or humans were protected from yellow fever infection. He went on to create the first safe and effective yellow fever vaccine in 1936, which he called 17D.
Theiler published results of his yellow fever vaccine trials in humans in 1937. The vaccine was approved and mass-produced that year, and quickly became the universal standard. Theiler would later win a Nobel Prize for his vaccine research.
Mass vaccination campaigns nearly eradicated the disease from some countries by 1961, but others continued to experience large outbreaks. Since the 1990s, there have been several yellow fever epidemics throughout Africa.
Influenza
British scientists Wilson Smith, Christopher Andrewes, and Patrick Laidlaw isolated the influenza virus in 1933 and began studying antibody production in ferrets.
Jonas Salk and Thomas Francis developed the first vaccine against influenza A in 1938. Two years later, Francis discovered influenza B, and the duo created a two-component flu vaccine in 1942.
The combined vaccine was first produced for military use in 1944, and then licensed for civilians in 1945 after testing on military recruits and college students.
But during the seasonal flu outbreak of 1947, researchers realized that new strains of influenza appear each year and require distinct vaccines. The WHO launched its first Influenza Centre in London in 1948, and centers around the world continue to research new vaccines today.
Measles, mumps, and rubella
American doctor Thomas Peebles first isolated the measles virus in February 1954, during an outbreak at a private school outside of Boston. His team tested the first version of the vaccine on 11 children with intellectual snd physical disabilities in 1958, and they found the virus in the vaccine was strong enough to give the kids some adverse symptoms.
After multiple rounds of reformulations and trials in Boston, John Enders finally licensed a vaccine that was safe and effective at preventing measles infections in 1963.
Merck's Maurice Hilleman developed a more attenuated vaccine in 1968, which he then combined with vaccines for mumps (licensed in 1967) and rubella (1969) to create the MMR vaccine in 1971. The combined vaccine induced immunity to all three viruses with no greater adverse reactions than a single vaccine.
The CDC aimed to eliminate the measles from the US with routine vaccinations starting in 1978, reaching success in 2000. However, cases from abroad have caused several small outbreaks in the 21st century.
Hepatitis B
Four years after discovering the virus, American physician and geneticist Baruch Blumberg developed the first hepatitis B vaccine in 1969 using an antigen he found in Australia. He later won a Nobel Prize for his research.
In 1981, the FDA approved a more sophisticated vaccine derived from the blood of hepatitis B-positive donors, but it was discontinued in 1990 due to fears surrounding the AIDS epidemic.
Researchers developed a vaccine made from genetically engineered DNA in 1986. This vaccine, which is still used today, does not contain blood products and cannot get people sick with hepatitis B.
Chickenpox
In 1974, Michiaki Takahashi isolated the "Oka" strain of varicella, or chickenpox, from a three-year-old boy in Japan. He developed a live attenuated chickenpox vaccine that same year and tested it on 23 children in hospital. All of the children who received the vaccine developed antibodies and did not fall ill despite an outbreak in their ward.
Clinical trials continued in Japan through 1986, when the vaccine was approved and rolled out for voluntary use.
The chickenpox vaccine was licensed in the US in 1995 and added to the child vaccine schedule, making the US the first country to introduce routine varicella vaccination for young children.
Swine flu
The first human infection with the new influenza A H1N1 virus was detected on April 15, 2009. The US CDC publicly reported the first two cases and announced vaccine research efforts were underway on April 21.
Clinical trials testing H1N1 flu vaccine candidates officially began on July 22. The FDA approved four vaccines on September 15.
The US placed its first vaccine orders two weeks later, and the US national H1N1 flu vaccination campaign officially launched in October. However, there were initial vaccine shortages and the vaccine wasn't widely available until December. Studies on the long-term safety of the vaccine continued to publish results through the end of the year.
COVID-19
Reports of a mysterious pneumonia outbreak in Wuhan, China, reached the WHO in early December 2019. It turned out the illness, now known as COVID-19, was a disease caused by a novel coronavirus, dubbed SARS-CoV-2, Chinese authorities reported January 7.
On March 16, 2020 — five days after the WHO declared a pandemic — Moderna was the first company to begin coronavirus vaccine safety trials. Several other companies launched their own trials shortly after, and there will likely be more than 50 coronavirus vaccine candidates in human testing by the end of the year.
Both Moderna and Pfizer announced preliminary positive results of their trials in November. Once their safety data are complete, they'll apply for emergency use authorization by the FDA.
If either or both candidates are approved, rollout will likely begin in the last days of 2020 or early 2021. Frontline workers and vulnerable populations will be eligible for vaccinations first, and the general public will likely have to wait until summer for a vaccine to be widely available.

